The History and Evolution of Psychiatry
Psychiatry, as a medical specialty, has a rich and complex history that spans centuries. Its evolution reflects the changing understanding of mental health and illness, shaped by scientific advancements, cultural shifts, and societal attitudes. This article delves into the historical development of psychiatry, exploring key milestones and transformations that have shaped the field into what it is today.
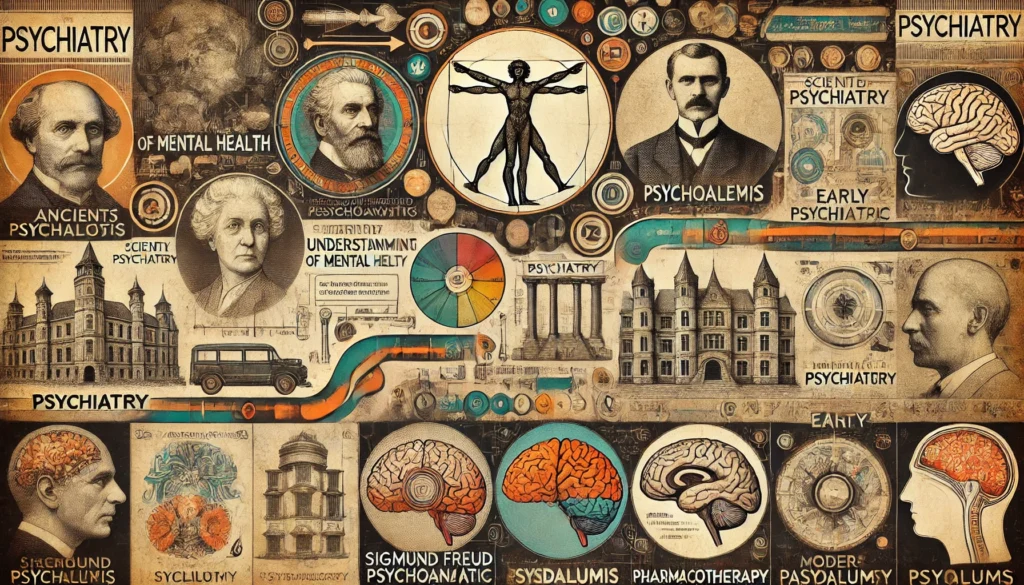
Ancient and Medieval Perspectives on Mental Health
The origins of psychiatry can be traced back to ancient civilizations, where mental illness was often viewed through a supernatural lens. In ancient Egypt, Greece, and Rome, mental disorders were attributed to the displeasure of gods or possession by evil spirits. Treatments during this time were largely based on religious rituals, exorcisms, and trephination—a practice involving drilling holes into the skull to release evil spirits.
Hippocrates, a Greek physician known as the “Father of Medicine,” was one of the first to propose a more naturalistic approach to mental health. He suggested that mental disorders were the result of imbalances in bodily fluids or “humors.” Hippocrates’ humoral theory laid the groundwork for later medical models, emphasizing the importance of physical and environmental factors in mental health. Despite this early scientific approach, supernatural explanations for mental illness persisted for centuries.
During the Middle Ages, the understanding of mental health regressed, largely influenced by the dominance of the Church. Mental illness was again seen as a manifestation of sin, demonic possession, or witchcraft. Treatments were often brutal, including imprisonment, exorcism, and even execution. Mentally ill individuals were frequently isolated in asylums or madhouses, where they were subjected to inhumane conditions and treatments.
The Renaissance period marked the beginning of a slow shift towards more humane treatments. Influential figures like Paracelsus, a Swiss physician, challenged the prevailing views of mental illness. He argued that mental disorders had natural causes and should be treated with compassion and care. Despite these emerging ideas, it would take several more centuries for significant changes in the treatment of mental illness to occur.
The Enlightenment era in the 17th and 18th centuries brought further advancements in the understanding of mental health. Philosophers and physicians began to advocate for more humane treatment of the mentally ill. Institutions known as “moral treatment” asylums were established, emphasizing kindness, structured activities, and better living conditions for patients. This period marked the beginning of a more scientific and compassionate approach to mental health care.
The Birth of Modern Psychiatry
The 19th century witnessed the formalization of psychiatry as a medical discipline. Pioneers such as Philippe Pinel in France and William Tuke in England played crucial roles in transforming the care of the mentally ill. Pinel, often regarded as the father of modern psychiatry, famously unchained patients at the Bicêtre Hospital in Paris and introduced more humane treatments based on observation and classification of mental disorders.
In England, William Tuke founded the York Retreat, a Quaker-run institution that implemented the principles of moral treatment. Patients at the York Retreat were treated with dignity, encouraged to engage in meaningful activities, and provided with a supportive environment. These reforms laid the foundation for the development of therapeutic communities and modern psychiatric hospitals.
The late 19th and early 20th centuries saw significant advancements in the classification and diagnosis of mental disorders. Emil Kraepelin, a German psychiatrist, developed a comprehensive system for categorizing mental illnesses, which influenced the development of the Diagnostic and Statistical Manual of Mental Disorders (DSM) used today. Kraepelin’s work emphasized the biological and genetic basis of mental illness, paving the way for future research in psychiatric genetics.
Sigmund Freud, an Austrian neurologist, revolutionized the field with his theories on psychoanalysis. Freud’s work focused on the unconscious mind, childhood experiences, and the role of repressed emotions in mental illness. While many of Freud’s theories have been criticized and revised, his emphasis on the psychological aspects of mental health had a profound impact on the field of psychiatry and the development of psychotherapeutic techniques.
The early 20th century also saw the rise of biological psychiatry, with researchers exploring the role of brain chemistry and physiology in mental disorders. The discovery of the first antipsychotic drug, chlorpromazine, in the 1950s revolutionized the treatment of schizophrenia and other severe mental illnesses. This breakthrough marked the beginning of the psychopharmacological era, where medications became a central component of psychiatric treatment.
The establishment of the National Institute of Mental Health (NIMH) in the United States in 1949 further propelled research and advancements in psychiatry. The NIMH played a crucial role in funding studies, developing new treatments, and promoting public awareness of mental health issues. This period also saw the deinstitutionalization movement, which aimed to transition patients from long-term psychiatric hospitals to community-based care settings.
Advances in Psychiatric Treatment and Research
The latter half of the 20th century and the early 21st century witnessed remarkable advancements in psychiatric treatment and research. The development of new psychotropic medications, such as selective serotonin reuptake inhibitors (SSRIs) for depression and atypical antipsychotics for schizophrenia, significantly improved the management of mental health conditions. These medications offered better efficacy and fewer side effects compared to earlier treatments.
Psychotherapy also evolved during this period, with the emergence of various therapeutic modalities. Cognitive-behavioral therapy (CBT), developed by Aaron Beck, became a widely used and evidence-based approach for treating depression, anxiety, and other mental disorders. CBT focuses on identifying and changing negative thought patterns and behaviors, helping patients develop healthier coping strategies.
Advances in neuroscience and neuroimaging techniques, such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), have deepened our understanding of the brain’s role in mental illness. These technologies allow researchers to study brain activity, structure, and function, leading to new insights into the biological basis of mental disorders. For example, studies have shown that individuals with depression often have altered brain activity in regions involved in mood regulation.
The integration of genetics into psychiatric research has also been transformative. The identification of specific genes associated with mental health conditions has opened new avenues for understanding the hereditary aspects of these disorders. Genome-wide association studies (GWAS) have identified genetic variants linked to conditions like schizophrenia, bipolar disorder, and autism, providing valuable insights into their etiology.
The rise of digital mental health tools and telepsychiatry has further expanded access to psychiatric care. Online therapy platforms, mobile apps for mental health, and telepsychiatry services have made it easier for individuals to receive treatment, especially in underserved areas. These digital innovations have been particularly valuable during the COVID-19 pandemic, ensuring continuity of care while minimizing the risk of virus transmission.
Statistical data underscores the impact of these advancements. According to the World Health Organization (WHO), the global prevalence of mental health disorders remains high, with approximately 1 in 4 people experiencing a mental health condition at some point in their lives. Despite this, the availability of effective treatments has improved outcomes for many individuals. For instance, the introduction of SSRIs has led to significant reductions in symptoms for approximately 60-70% of patients with major depressive disorder.
The Future of Psychiatry
The future of psychiatry holds promise for continued advancements in treatment, technology, and integration with other medical disciplines. As our understanding of mental health deepens and societal awareness grows, the field of psychiatry is poised to make even more significant contributions to healthcare and well-being.
One key area of future development in psychiatry is the focus on personalized medicine. Advances in genetics, neuroimaging, and artificial intelligence (AI) will enable more tailored and precise treatments for mental health conditions. Personalized medicine approaches consider an individual’s genetic makeup, brain structure, and environmental factors to develop targeted interventions. This approach promises to improve treatment efficacy and reduce side effects, leading to better patient outcomes.
Preventive psychiatry will also become increasingly important. Early identification and intervention for mental health conditions can prevent the progression of symptoms and reduce the overall burden of mental health disorders. Public health initiatives, mental health screenings, and community outreach programs will play a vital role in promoting early detection and intervention. Psychiatrists will continue to be at the forefront of these efforts, working to reduce the prevalence and impact of mental health conditions.
The integration of mental health care into primary care settings will likely expand, improving access to psychiatric services and promoting holistic care. Collaborative care models, where primary care physicians and psychiatrists work together to manage patients’ overall health, will become more prevalent. This integration ensures that mental health is considered an essential component of comprehensive healthcare.
Advancements in digital mental health will also shape the future of psychiatry. Telepsychiatry, digital therapeutics, and AI-driven tools will continue to enhance access to care and improve treatment outcomes. These technologies provide new ways for patients to engage with mental health services and receive support. As digital mental health tools become more sophisticated, they will offer increasingly effective and personalized interventions.
The future of psychiatry will also see greater recognition of the social determinants of mental health. Factors such as socioeconomic status, education, and community environment significantly impact mental health outcomes. Addressing these social determinants through policy changes, community programs, and advocacy will be essential for promoting mental well-being. Psychiatrists will play a key role in these efforts, working to create supportive environments that foster mental health.
At Lumende, we understand the critical role that psychiatry plays in modern medicine and the importance of staying at the forefront of these advancements. Our platform connects individuals with experienced psychiatrists and mental health professionals who provide personalized and comprehensive care. Through online therapy sessions,we offer accessible and effective psychiatric support to help individuals achieve better mental health and well-being.

 English
English
 Deutsch
Deutsch Français
Français