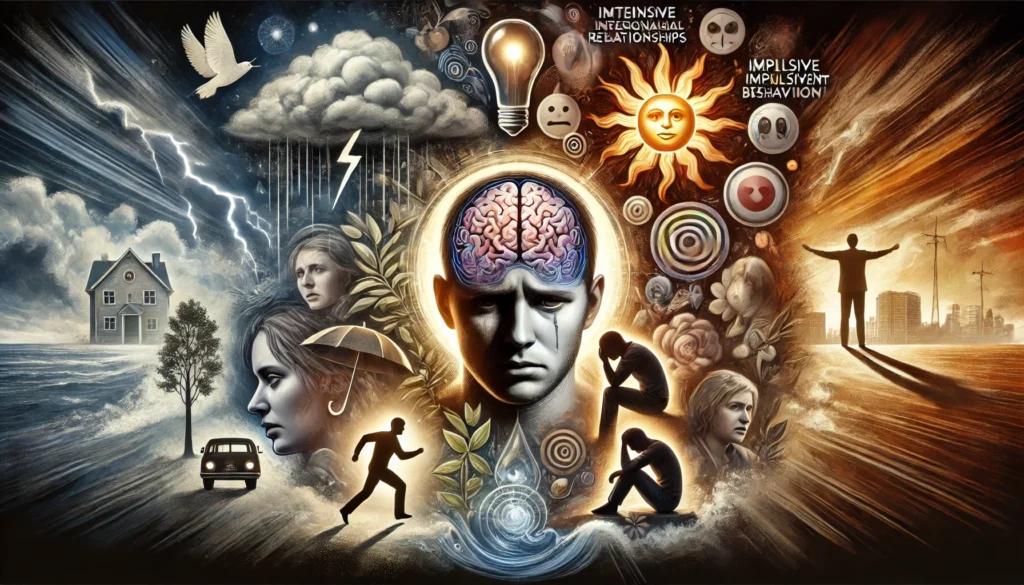
Navigating Life with Borderline Personality Disorder
Borderline Personality Disorder (BPD) is a complex mental health condition characterized by emotional instability, intense interpersonal relationships, and impulsive behavior. Navigating life with BPD can be challenging, but understanding the disorder and exploring effective management strategies can help individuals lead fulfilling lives. This article delves into the various aspects of living with BPD, offering insights and practical advice for those affected by the condition.
Understanding Borderline Personality Disorder
Borderline Personality Disorder is marked by a pervasive pattern of instability in emotions, self-image, and interpersonal relationships. Individuals with BPD often experience intense episodes of anger, depression, and anxiety that can last from a few hours to several days. These emotional fluctuations can be overwhelming and lead to impulsive actions and relationship turmoil. This instability can be particularly difficult to manage, as it often occurs without a clear trigger, making it hard for those affected to predict or control their mood swings.
One of the hallmarks of BPD is fear of abandonment. Individuals with BPD may go to great lengths to avoid real or perceived abandonment, including impulsive actions such as self-harm or threats of suicide. This intense fear often stems from early childhood experiences of instability or neglect. According to the National Institute of Mental Health (NIMH), around 1.4% of adults in the United States are affected by BPD, with the condition being more commonly diagnosed in women than in men.
Another key feature of BPD is an unstable self-image. Individuals with BPD may have difficulty maintaining a consistent sense of self, often feeling unsure about their identity and values. This can lead to frequent changes in interests, goals, and careers. This identity disturbance contributes to feelings of emptiness and can exacerbate emotional instability.
Interpersonal relationships are often turbulent for individuals with BPD. They may experience intense and unstable relationships characterized by alternating between extremes of idealization and devaluation. This pattern, known as splitting, can cause significant distress and misunderstandings in relationships. For example, a person with BPD might initially idolize a new friend or partner, only to later become disillusioned and angry over minor perceived slights.
Impulsivity is another significant aspect of BPD. This can manifest in various ways, such as reckless driving, binge eating, substance abuse, or risky sexual behavior. These impulsive actions are often attempts to manage emotional pain or fill a perceived void. Unfortunately, these behaviors can lead to further complications, such as legal issues, financial problems, and strained relationships. Impulsivity can also endanger the individual’s physical health and safety, creating additional challenges in their daily life and exacerbating feelings of guilt and regret.
Chronic feelings of emptiness and inappropriate, intense anger are additional symptoms of BPD. Individuals with BPD may feel a pervasive sense of boredom or emptiness, seeking stimulation through impulsive or risky behaviors. Anger in BPD can be intense and difficult to control, often leading to physical altercations or aggressive outbursts. This anger can be particularly damaging in relationships, as it can result in hurtful words or actions that are difficult to repair, further isolating the individual and reinforcing their fears of abandonment and rejection.
Understanding these symptoms is the first step toward managing BPD. Recognizing the patterns and triggers that contribute to emotional instability can help individuals develop strategies to cope with the disorder. Professional support from therapists and psychiatrists is critical in this process, offering guidance and treatment options tailored to the individual’s needs.
Therapeutic Approaches for BPD
Effective treatment for BPD involves a combination of therapeutic approaches designed to address the complex and multifaceted nature of the disorder. Dialectical Behavior Therapy (DBT) is one of the most effective and widely used treatments for BPD. Developed by Dr. Marsha Linehan, DBT focuses on teaching skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. These skills are taught through a combination of individual therapy sessions and skills training groups, providing a comprehensive approach to managing the symptoms of BPD.
Distress tolerance skills teach individuals how to cope with and tolerate distressing situations without resorting to self-destructive behaviors. Techniques such as radical acceptance, self-soothing, and distraction can help individuals manage intense emotions. For instance, if someone with BPD feels overwhelmed by sadness, they might use a distress tolerance skill like taking a cold shower or engaging in a hobby to divert their attention and calm their emotions.
Emotion regulation skills are crucial for individuals with BPD, as they often struggle with intense and rapidly changing emotions. DBT teaches techniques to identify, understand, and manage emotions effectively. This might involve keeping an emotion diary, practicing opposite action (engaging in an activity opposite to the emotion’s urge), or improving emotional literacy.
Interpersonal effectiveness skills focus on improving communication and relationship-building abilities. Individuals with BPD learn how to assert their needs, set boundaries, and navigate conflicts constructively. For example, someone with BPD might practice using “I” statements to express their feelings without blaming others, which can help reduce misunderstandings and build healthier relationships.
Schema Therapy is another therapeutic approach that can be beneficial for individuals with BPD. This therapy combines elements of cognitive-behavioral therapy, psychoanalysis, and attachment theory to help individuals understand and change deeply ingrained patterns of thinking and behavior. Schema Therapy focuses on identifying and addressing maladaptive schemas, which are negative beliefs about oneself and the world formed in childhood.
Mentalization-Based Therapy (MBT) is also effective in treating BPD. MBT helps individuals improve their ability to understand and interpret their own and others’ mental states, such as thoughts, feelings, and intentions. This improved mentalization can enhance empathy, reduce misunderstandings, and improve emotional regulation. For example, MBT might help someone with BPD recognize that a friend’s lack of response to a text message is not necessarily a sign of rejection, but rather could be due to the friend being busy.
Medication and Medical Interventions
While therapy is a cornerstone of BPD treatment, medication can also play a role in managing specific symptoms. It’s important to note that there is no medication specifically approved to treat BPD. However, medications can be prescribed to address co-occurring conditions or specific symptoms such as mood swings, depression, anxiety, or impulsivity. A tailored medication regimen, combined with therapy, can provide comprehensive support for individuals with BPD.
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), are often prescribed to manage symptoms of depression and anxiety in individuals with BPD. SSRIs can help stabilize mood and reduce feelings of sadness and hopelessness. For instance, someone with BPD who experiences chronic depression might benefit from an SSRI like fluoxetine or sertraline. These medications can help alleviate the emotional burden and improve overall functioning, making it easier for individuals to engage in therapeutic interventions.
Mood stabilizers, such as lithium or valproate, can help control mood swings and reduce impulsive behaviors. These medications can be particularly helpful for individuals with BPD who experience intense emotional highs and lows. For example, a person with BPD who frequently oscillates between extreme anger and depression might find relief with a mood stabilizer.
Antipsychotic medications can be beneficial for individuals with BPD who experience severe anxiety, paranoia, or dissociation. Low doses of antipsychotics like quetiapine or aripiprazole can help manage these symptoms and improve overall functioning. For instance, someone with BPD who struggles with paranoia might experience fewer paranoid thoughts with the help of an antipsychotic medication.
In some cases, benzodiazepines may be prescribed for short-term relief of severe anxiety or agitation. However, due to the risk of dependency and potential for misuse, benzodiazepines are typically used with caution and for limited periods. For example, a person with BPD experiencing an acute anxiety episode might be prescribed a short course of a benzodiazepine like lorazepam to manage immediate symptoms.
Individuals with BPD must work closely with their healthcare providers to find the right medication regimen. Medication management often involves a process of trial and error to determine the most effective medications and dosages. Regular follow-up appointments are essential to monitor progress, manage side effects, and make any necessary adjustments to the treatment plan.
In addition to medication, some individuals with BPD may benefit from other medical interventions such as Transcranial Magnetic Stimulation (TMS) or Electroconvulsive Therapy (ECT). TMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain, which can help improve symptoms of depression. ECT, although more invasive, can be effective for severe depression that does not respond to other treatments. Both TMS and ECT should be considered as part of a comprehensive treatment plan and discussed thoroughly with a healthcare provider.
Navigating Daily Life with BPD
Living with BPD can be challenging, but with the right strategies and support, individuals can navigate daily life more effectively. Developing a structured routine can provide stability and predictability, which can help manage emotional fluctuations. This might include setting regular times for waking up, eating, exercising, and going to bed. A consistent routine can create a sense of order and control, reducing the impact of chaotic emotions on daily life.
Building a strong support network is crucial for individuals with BPD. Trusted friends, family members, and mental health professionals can provide emotional support, encouragement, and practical assistance. Open and honest communication with loved ones about BPD and its impact can foster understanding and reduce misunderstandings. For example, explaining to a friend that sudden mood swings are part of the disorder, not a reflection of their relationship, can help maintain supportive friendships. A robust support system can also offer a safety net during times of crisis, providing immediate assistance and reassurance.
Engaging in self-care activities is essential for managing BPD symptoms. This can include hobbies, exercise, relaxation techniques, and spending time in nature. Finding activities that bring joy and relaxation can help individuals cope with stress and improve their overall well-being. For instance, someone with BPD might find that regular yoga practice helps them feel more grounded and centered.
Learning to manage stress effectively is also crucial for individuals with BPD. High levels of stress can exacerbate symptoms and lead to impulsive behaviors. Stress management techniques such as deep breathing exercises, progressive muscle relaxation, and guided imagery can help reduce stress levels. Additionally, finding healthy outlets for emotions, such as journaling or talking with a trusted friend, can be beneficial.
Setting realistic goals and celebrating small achievements can boost self-esteem and provide a sense of accomplishment. For individuals with BPD, breaking down larger tasks into smaller, manageable steps can make them feel less overwhelming. For example, if someone with BPD wants to improve their physical fitness, they might start with short daily walks and gradually increase the duration and intensity of their workouts.
At Lumende, we understand the complexities of navigating life with Borderline Personality Disorder and the importance of comprehensive support. Our platform connects individuals with experienced psychologists and psychiatrists who specialize in treating BPD and related conditions. Through personalized online therapy sessions, we help individuals develop effective strategies for managing symptoms, improving their mental health, and enhancing their quality of life. Our goal is to provide ongoing support and resources to help individuals achieve lasting well-being and recovery.

 English
English
 Deutsch
Deutsch Français
Français