The Impact of Alzheimer’s on Memory and Daily Functioning
Alzheimer’s disease, a progressive neurological disorder, profoundly impacts memory and daily functioning. As the most common cause of dementia, Alzheimer’s affects millions of people worldwide, gradually eroding cognitive abilities and interfering with everyday activities. Understanding how Alzheimer’s influences memory and daily functioning is essential for caregivers and loved ones, as it allows for better preparation and management of the disease.
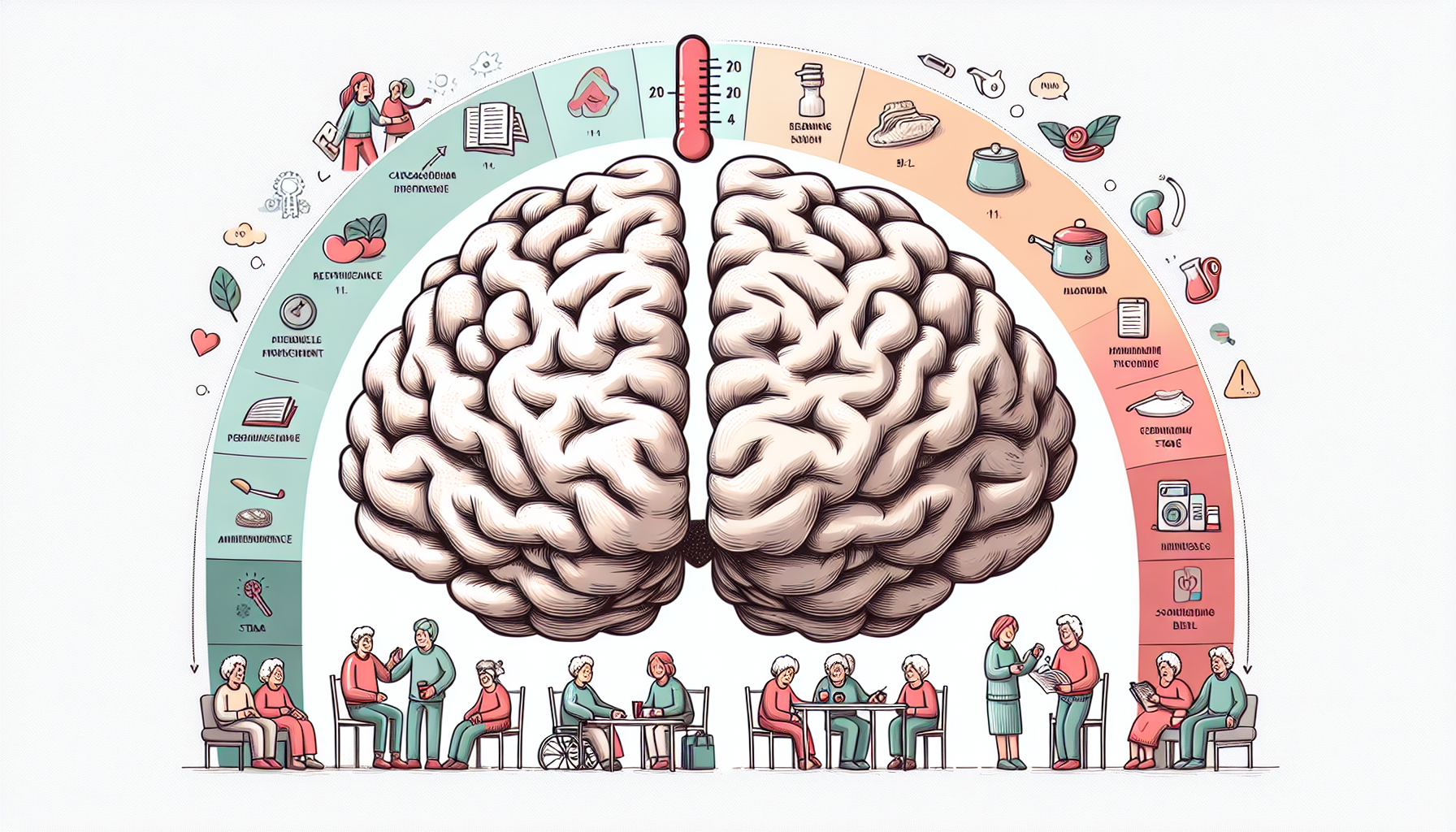
How Alzheimer’s Affects Memory
One of the earliest and most recognizable symptoms of Alzheimer’s disease is memory loss. This memory impairment typically starts with difficulty in recalling recent events or newly acquired information. Individuals might struggle to remember important dates, appointments, or conversations they had just a short while ago. Unlike normal age-related memory lapses, these memory problems are persistent and progressively worsen over time.
As the disease advances, the ability to form new memories deteriorates significantly. This condition, known as anterograde amnesia, means that individuals find it increasingly difficult to learn new information or skills. They may repeatedly ask the same questions, not because they are inattentive, but because they cannot retain the answers provided to them.
Additionally, Alzheimer’s affects long-term memory, leading to the erosion of memories that were previously well-established. Personal history, relationships, and significant life events can become hazy or forgotten entirely. This loss of personal history can be deeply distressing for both the individual and their loved ones, as it affects their sense of identity and connection to the past.
Moreover, semantic memory, which encompasses the understanding of facts and general knowledge about the world, also deteriorates. Individuals may forget common facts, such as the names of everyday objects or the functions of household items. This can lead to confusion and frustration, making routine activities more challenging.
Working memory, the ability to hold and manipulate information over short periods, is similarly impaired. This affects the capacity to follow conversations, keep track of tasks, or make decisions based on immediate information. For instance, someone with Alzheimer’s may struggle to follow the steps of a recipe or forget what they were doing in the middle of a task.
According to the Alzheimer’s Association, approximately 5.8 million Americans are living with Alzheimer’s disease, with one in ten people aged 65 and older affected. This statistic underscores the widespread impact of the disease on memory and highlights the importance of recognizing and addressing these cognitive changes early.
Daily Functioning Challenges
Alzheimer’s disease not only impairs memory but also significantly disrupts daily functioning. As cognitive abilities decline, individuals find it increasingly difficult to perform routine tasks that once came naturally. These challenges can vary widely depending on the stage of the disease and the specific areas of the brain that are affected.
One of the primary areas affected is executive functioning, which includes planning, organizing, and executing tasks. Individuals may struggle to manage their finances, follow multi-step instructions, or adhere to schedules. This can lead to missed appointments, unpaid bills, and a general sense of disorganization.
Personal care routines, such as bathing, dressing, and grooming, also become challenging. Individuals might forget to perform these tasks, perform them inadequately, or require step-by-step guidance. This decline in personal hygiene and self-care can significantly affect their overall well-being and quality of life.
Household chores and maintenance activities often become overwhelming. Tasks such as cooking, cleaning, and laundry require a level of organization and memory that can be difficult to maintain. Individuals may leave stoves on, forget to clean, or be unable to manage the complexities of household appliances.
Driving is another area of daily functioning that is heavily impacted by Alzheimer’s disease. Navigating familiar routes can become confusing, and individuals may get lost easily. Their reaction times and decision-making abilities also decline, making driving potentially dangerous. For many, giving up driving represents a significant loss of independence and freedom.
Social interactions and relationships are also affected. Individuals may withdraw from social activities they once enjoyed due to difficulties in following conversations or remembering names and faces. This withdrawal can lead to isolation and depression, exacerbating the emotional toll of the disease.
Additionally, the ability to engage in leisure activities, such as hobbies or sports, diminishes. The cognitive processes required for these activities, including attention, memory, and problem-solving, are often impaired. This loss can lead to a decline in overall mental and physical health, as well as a reduction in the quality of life.
Behavioral and Psychological Symptoms
In addition to memory and functional impairments, Alzheimer’s disease often leads to various behavioral and psychological symptoms. These changes can be particularly distressing for both individuals and their caregivers, as they add complexity to the management of the disease.
One common symptom is increased agitation and irritability. Individuals may become easily frustrated or upset, often over seemingly minor issues. This can lead to outbursts of anger or aggressive behavior, which can be challenging for caregivers to manage.
Depression and anxiety are also prevalent among those with Alzheimer’s. The awareness of cognitive decline and the resultant loss of independence can lead to significant emotional distress. These mood changes can further complicate the disease’s management and negatively impact the individual’s quality of life.
Paranoia and delusions are other potential symptoms. Individuals may develop unfounded beliefs, such as thinking that others are stealing from them or that their spouse is unfaithful. These delusions can strain relationships and make caregiving more difficult.
Hallucinations, although less common, can occur, particularly in the later stages of the disease. Individuals may see or hear things that are not present, which can be frightening and confusing. Managing these symptoms requires patience and understanding from caregivers and healthcare professionals.
Sleep disturbances are also frequent. Individuals with Alzheimer’s may experience changes in their sleep patterns, such as difficulty falling asleep, waking frequently during the night, or sleeping excessively during the day. These disruptions can lead to increased fatigue and exacerbate other symptoms.
Wandering is a particularly concerning behavior associated with Alzheimer’s. Individuals may become disoriented and attempt to leave their homes, leading to safety risks. Caregivers need to take precautions to ensure the individual’s safety, such as installing alarms or using GPS tracking devices.
When to Seek Help
Recognizing when to seek professional help is crucial for managing Alzheimer’s disease effectively. Early intervention can improve the quality of life for individuals and provide much-needed support for caregivers. There are several key indicators that it may be time to seek help.
One noticeable sign is the escalation of memory problems. If memory loss begins to interfere with daily life significantly, such as forgetting important dates, appointments, or events regularly, it’s time to consult a healthcare professional. An accurate diagnosis can provide a clearer understanding of the situation and inform appropriate interventions.
Behavioral changes that are persistent and concerning should also prompt a visit to the doctor. This includes increased agitation, paranoia, or depression that affects the individual’s ability to function. A professional evaluation can help determine if these behaviors are related to Alzheimer’s or another condition that may require different treatment.
Difficulties in performing daily tasks are another red flag. If the individual is struggling with activities like managing finances, personal care, or household chores, it may indicate a decline in cognitive function that warrants medical attention. Assessing these changes can help in planning for the necessary support and care.
Social withdrawal and changes in interpersonal relationships are also significant. If the person begins to isolate themselves from friends and family, it may be a sign that they are experiencing difficulties in social interactions due to cognitive decline. Addressing these changes early can help maintain social connections and prevent isolation.
Safety concerns, such as getting lost while driving or wandering away from home, are critical indicators. If there is a risk to the individual’s safety or the safety of others, it’s essential to seek help immediately. Professional guidance can provide strategies to manage these risks effectively.
Finally, if caregivers are feeling overwhelmed, it’s crucial to seek support. Caring for someone with Alzheimer’s can be demanding, and professional assistance can provide respite and ensure that the caregiver’s well-being is also addressed.
At Lumende, we offer comprehensive support for individuals with Alzheimer’s disease and their caregivers. Our platform connects you with experienced mental health professionals who can provide personalized care and guidance. Whether you need help with diagnosis, managing symptoms, or coping strategies, Lumende is here to support you every step of the way.

 English
English
 Deutsch
Deutsch Français
Français