The Psychology Behind Anorexia and Bulimia: Causes and Treatments
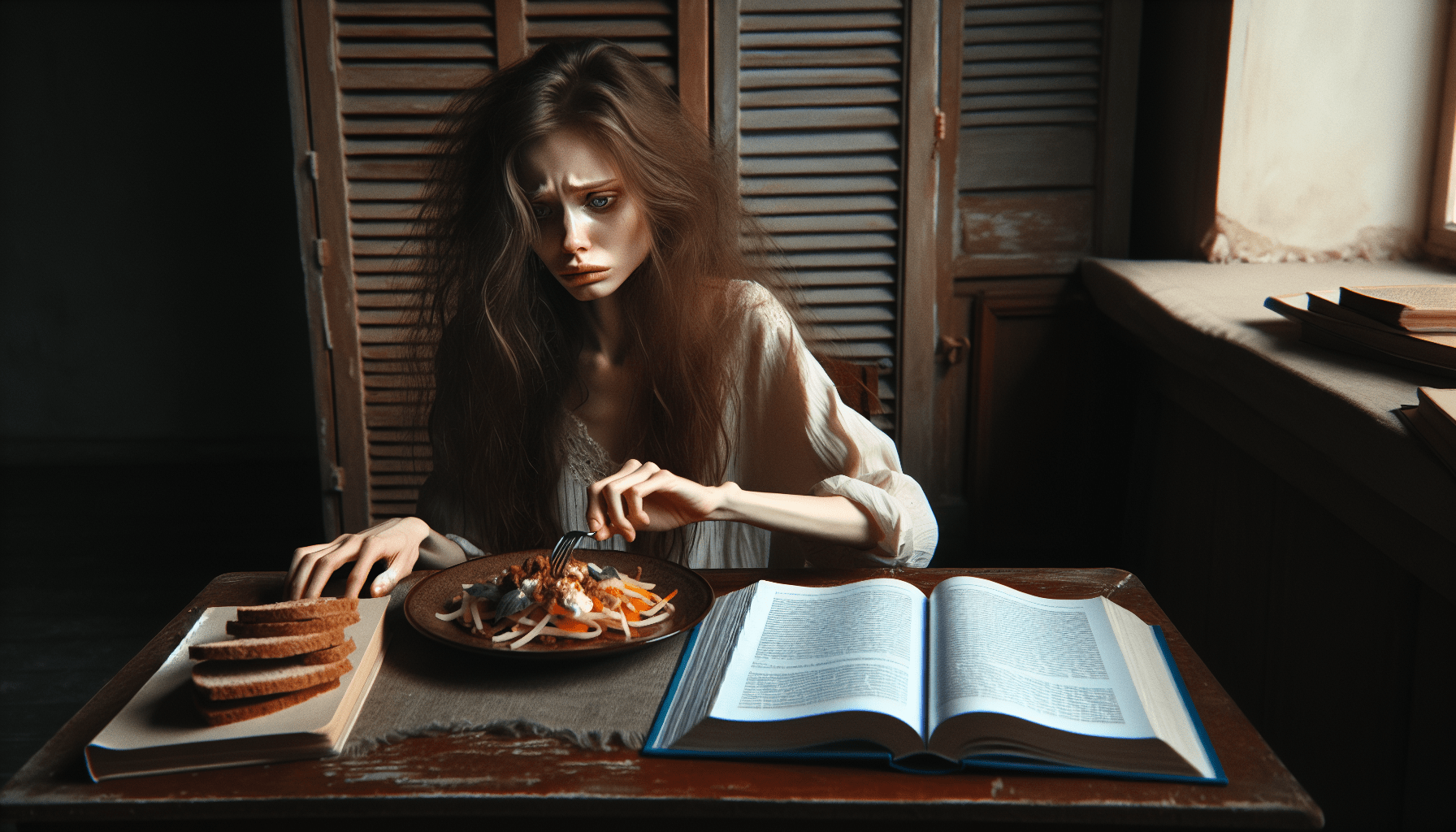
Understanding the psychology behind anorexia nervosa and bulimia nervosa is crucial for identifying effective treatments and providing appropriate support. These eating disorders, which are complex and multifaceted, stem from a variety of psychological, biological, and sociocultural factors. This section explores the underlying causes and the psychological aspects of these disorders, offering insights into their development and persistence.
Psychological Causes of Anorexia and Bulimia
The psychological factors contributing to anorexia and bulimia are diverse and intricate. One significant aspect is the presence of underlying mental health issues. Many individuals with eating disorders also struggle with anxiety, depression, obsessive-compulsive disorder (OCD), or trauma. These co-occurring conditions can exacerbate the symptoms of eating disorders and complicate their treatment.
Perfectionism is another common psychological trait among individuals with anorexia and bulimia. Perfectionists set extremely high standards for themselves and are highly self-critical when they perceive they have failed to meet these standards. This relentless pursuit of perfection can manifest in the need to maintain an unrealistically low body weight or engage in compulsive eating and purging behaviors.
Low self-esteem and a distorted body image are central to both anorexia and bulimia. Individuals with these disorders often have a deep-seated dissatisfaction with their bodies, which is not alleviated by weight loss or other measures. This body dissatisfaction is perpetuated by negative self-talk and unrealistic comparisons to others, often fueled by media and societal standards of beauty.
Control is a crucial element in the psychological landscape of eating disorders. For many individuals, controlling their food intake or body weight provides a sense of control that they feel is lacking in other areas of their lives. This perceived control can become addictive, leading to increasingly extreme behaviors to maintain this sense of order.
Trauma and stress also play significant roles in the development of eating disorders. Traumatic experiences, such as physical or sexual abuse, can lead individuals to use food as a coping mechanism, either through restrictive eating or bingeing and purging. Additionally, high levels of stress, whether from personal relationships, academic pressure, or societal expectations, can trigger or worsen symptoms of anorexia and bulimia.
Finally, family dynamics and upbringing can influence the development of eating disorders. Families that place a high value on appearance, weight, or achievement may inadvertently contribute to the development of unhealthy eating behaviors. Additionally, individuals who grow up in environments where food is used as a reward or punishment may develop distorted relationships with food and body image.
Biological and Genetic Factors
While psychological factors are significant, biological and genetic components also play crucial roles in the development of anorexia and bulimia. Research indicates that these disorders often run in families, suggesting a genetic predisposition. Studies involving twins have shown that if one twin has an eating disorder, the other twin is more likely to develop one as well, highlighting the genetic link.
Neurobiological factors also contribute to eating disorders. Abnormalities in brain structure and function, particularly in areas related to appetite regulation, mood, and impulse control, have been observed in individuals with anorexia and bulimia. For example, serotonin, a neurotransmitter involved in mood regulation, is often found to be imbalanced in those with eating disorders. This imbalance can lead to obsessive behaviors and a heightened sensitivity to environmental stressors.
Hormonal imbalances may also play a role. Hormones that regulate hunger and satiety, such as leptin and ghrelin, can be disrupted in individuals with eating disorders. These hormonal imbalances can affect appetite and metabolism, perpetuating the cycle of restrictive eating or bingeing and purging.
Additionally, the reward pathways in the brain, which involve dopamine, are implicated in eating disorders. Food can trigger the release of dopamine, creating feelings of pleasure and reward. For individuals with bulimia, binge eating may become a way to self-soothe or escape negative emotions, while those with anorexia may derive a sense of reward from extreme control and restriction.
Genetic factors can also influence personality traits that predispose individuals to eating disorders. Traits such as impulsivity, emotional instability, and perfectionism can be inherited and may increase the risk of developing anorexia or bulimia. Understanding these genetic predispositions can help in developing personalized treatment plans that address the specific needs of each individual.
Finally, there is evidence that prenatal and perinatal factors may contribute to the risk of developing eating disorders. Complications during pregnancy or birth, such as maternal malnutrition or low birth weight, have been linked to a higher risk of eating disorders later in life. These early life factors may influence brain development and predispose individuals to mental health issues, including eating disorders.
Sociocultural Influences
Sociocultural factors significantly impact the development and maintenance of eating disorders. The media, societal norms, and cultural values play powerful roles in shaping individuals’ perceptions of beauty and body image, often promoting unrealistic and unattainable standards.
The pervasive influence of media cannot be overstated. Television, magazines, social media, and advertising frequently depict an idealized body type that is often thin and toned. These images can create pressure to conform to these standards, leading individuals to engage in extreme behaviors to achieve a similar appearance. Studies have shown that exposure to media portraying thin ideals is linked to body dissatisfaction and eating disorder symptoms.
Peer pressure and social comparisons also contribute to the development of eating disorders. Adolescents and young adults are particularly susceptible to peer influence, and social comparisons can lead to feelings of inadequacy and the desire to alter one’s body to fit in. This is especially true in environments where there is a strong emphasis on appearance, such as in certain sports, dance, or modeling industries.
Cultural attitudes toward food and eating play a significant role as well. In some cultures, thinness is highly valued and associated with success, self-control, and attractiveness. Conversely, in cultures where food is abundant and central to social gatherings, individuals may experience conflict between societal expectations and cultural practices, potentially leading to disordered eating behaviors.
Family and community attitudes toward weight and appearance can also impact the risk of developing an eating disorder. Families that emphasize dieting, weight control, or criticize physical appearance may inadvertently contribute to the development of unhealthy eating behaviors. Positive or negative comments about weight and body shape can significantly influence an individual’s self-esteem and body image.
The increasing prevalence of social media has introduced new dynamics to sociocultural influences on eating disorders. Platforms like Instagram, TikTok, and Facebook allow for constant exposure to images of idealized bodies and lifestyles. The pressure to curate a perfect online persona can lead to unhealthy comparisons and the adoption of extreme dieting or exercise behaviors. According to a study by the Pew Research Center, 45% of teens feel overwhelmed by the pressure to present a perfect image on social media, which can exacerbate body image concerns and eating disorder symptoms.
Finally, societal stressors such as discrimination, bullying, and trauma can also contribute to the development of eating disorders. Individuals who experience weight-based bullying or discrimination due to their body size may internalize negative beliefs about themselves, leading to disordered eating as a coping mechanism. Addressing these broader societal issues is crucial for preventing eating disorders and promoting healthy body image and self-esteem.
Treatment Approaches for Anorexia and Bulimia
Effective treatment for anorexia and bulimia requires a comprehensive, multidisciplinary approach that addresses the physical, psychological, and social aspects of the disorders. Early intervention is critical, as it improves the likelihood of recovery and reduces the risk of long-term complications.
Cognitive-behavioral therapy (CBT) is one of the most effective treatments for eating disorders. CBT focuses on identifying and changing distorted thought patterns and behaviors related to food, body image, and self-esteem. This therapy helps individuals develop healthier coping mechanisms and establish a more balanced relationship with food. Studies have shown that CBT can significantly reduce symptoms of bulimia and is also effective for treating anorexia, particularly when combined with other therapeutic approaches.
Nutritional rehabilitation and counseling are essential components of treatment. Registered dietitians work with individuals to develop meal plans that restore physical health and normalize eating patterns. Nutritional counseling also addresses misconceptions about food and body image, helping individuals make informed, healthy choices. Restoring physical health is a crucial step in the recovery process, as malnutrition can impair cognitive function and exacerbate psychological symptoms.
Family-based therapy (FBT) is particularly effective for adolescents with eating disorders. FBT involves the entire family in the treatment process, empowering parents to take an active role in their child’s recovery. This approach helps to improve family communication, support the individual with the eating disorder, and address any familial dynamics that may contribute to the disorder. Research has shown that FBT can be highly effective in achieving remission in adolescent anorexia patients.
Medication can also play a role in treating eating disorders, particularly when co-occurring conditions such as depression or anxiety are present. Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), can help alleviate symptoms of depression and reduce binge-purge behaviors in bulimia. However, medication is generally most effective when combined with psychotherapy and other therapeutic interventions.
Support groups and peer support are valuable resources for individuals recovering from eating disorders. Connecting with others who have similar experiences can provide a sense of community and reduce feelings of isolation. Support groups offer a safe space to share challenges, successes, and coping strategies, fostering a supportive environment for recovery.
For those seeking specialized help, Lumende offers access to experienced mental health professionals who can provide personalized treatment plans for eating disorders. Whether through online therapy sessions, nutritional counseling, or support groups, Lumende’s resources can help individuals navigate their recovery journey and achieve lasting well-being. By leveraging the expertise available through Lumende, individuals with anorexia and bulimia can receive comprehensive care tailored to their unique needs, enhancing their chances of successful recovery.

 English
English
 Deutsch
Deutsch Français
Français